
How a Leading Insurance Service Provider Achieved 86% Success Rate in Settling Claims?


Challenges and Goals
A leading insurance firm with a customer base spanning lakhs of policy holders across the country, was facing operational difficulties in their claim settlement process. The company struggled to keep pace with rising volumes of claim inquiries and manual administrative workflows. The lack of automation in insurance claims and integrated systems not only slowed down claim settlements but also impacted customer satisfaction and overall service quality. These challenges highlighted an urgent need for the firm to integrate AI in insurance claim operations.
- High Volume of Claim Status Queries:- The client faced a surge in claim status inquiries, with service teams manually addressing each request. This led to slower responses and a poor customer experience in insurance claim processing.
- Manual Paperwork and Documentation:- Dependence on paper-based claim processing caused delays, misplaced documents, and compliance risks due to lack of digital claim management.
- Time-Consuming Claim Settlements:- Without workflow automation, claim settlements required multiple manual checks across departments, resulting in slow turnaround times and dissatisfied customers.
- Error-Prone Administrative Workflows:- Manual data entry and repetitive validation steps led to frequent errors, rework, and higher administrative costs.
Rezo’s Approach and Solution
Rezo AI’s goal was to automate the insurance claim settlement process. To achieve this, it leveraged its Agentic AI platform in the claim settlement process. The AI system provided fully autonomous information handling by automatically collecting and processing customer data, eliminating manual searches, and streamlining information retrieval for faster operations. Additionally, it enabled dynamic process navigation, intelligently managing complex workflows and adapting in real time to any changes in context or claim status, providing seamless execution. The platform also delivered personalized resolutions for each customer by learning from previous interactions, leading to improved accuracy and higher satisfaction over time. Thus, by automating tasks end-to-end, the AI system was able to achieve faster claim settlements in the shortest possible time and streamline contact center operations without any human intervention.
Rezo AI’s Approach to Claim Settlement: -
Rezo integrated its Agentic AI platform to automate the end-to-end insurance claim settlement process, streamlining every stage from claim identification to final settlement. This implementation transformed the firm’s operations through intelligent automation and adaptive process management.
Automated Claim Retrieval
The Agentic AI agents automatically fetched customers’ claim numbers, both single and multiple, from the ICAN database with complete accuracy. This automation eliminated manual lookups, reduced call drop rates, and improved overall customer engagement.
Intelligent Claim Status Mapping
It established intelligent mapping with different claim status stages, covering the entire journey from claim registration to claim closure. This ensured timely and accurate resolution of customer queries for insurance claim settlement.
Feedback and Resolution Tracking
Following each interaction, the AI system captured overall CSAT scores and generated First Time Resolution tickets. In cases where customers were not satisfied, it triggered response-based workflows to provide additional support and achieve complete resolution.
Smart Routing for Complex Cases
In instances where no claim number was found, Rezo’s Agentic AI platform for insurance claim automation routed calls to the relevant support executives for claim registration or complex queries. This approach delivered personalized resolutions while significantly reducing agent workload.
Results and Impact
After implementing Rezo AI’s Agentic AI platform for insurance claim settlement, the Insurance firm achieved a significant transformation in its claims management operations. By automating the entire claim settlement process from claim identification to final resolution, the firm was able to drastically reduce manual intervention and streamline customer interactions.
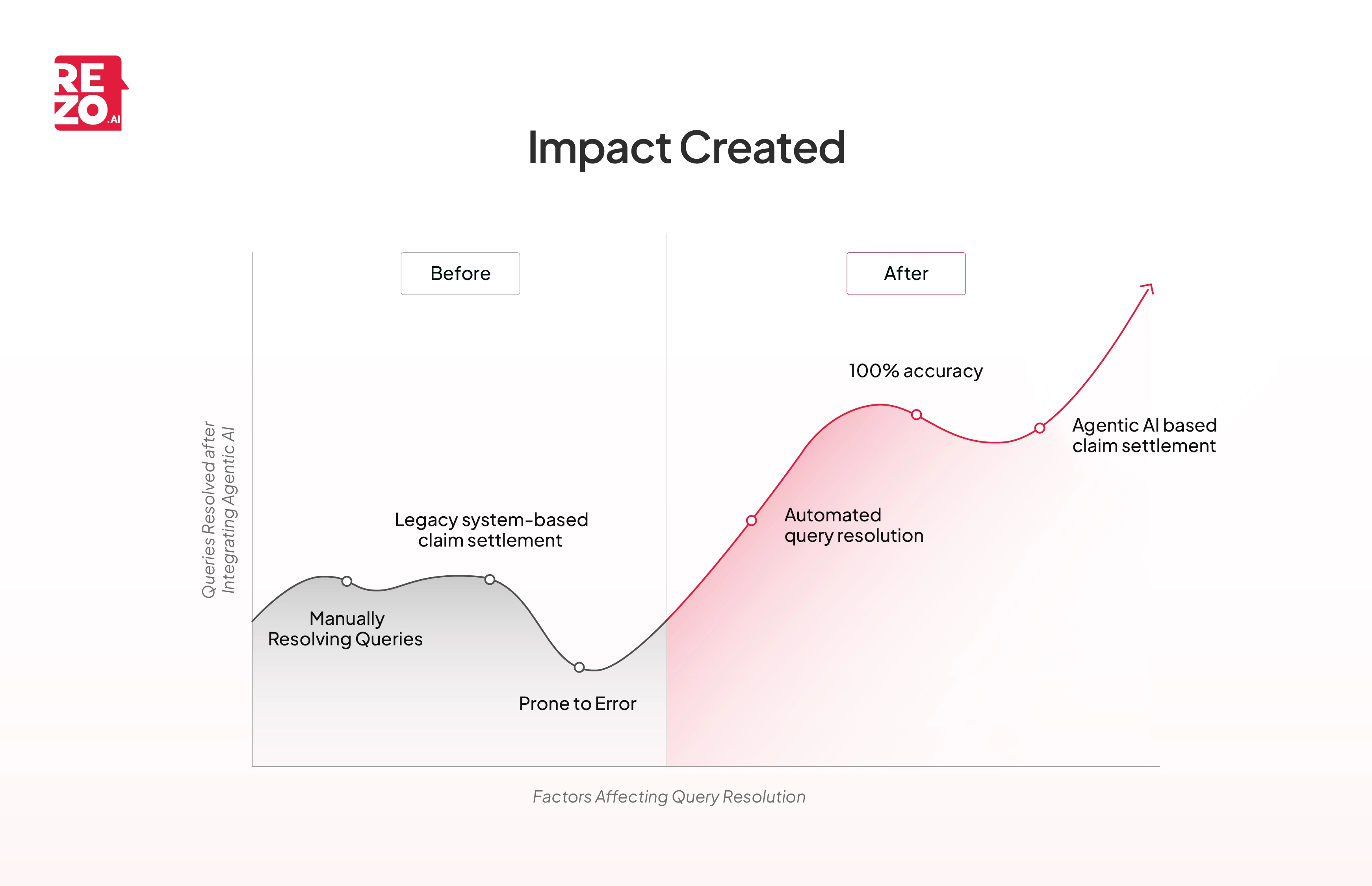
As a result, nearly 75% of customer calls were automated end to end, freeing up agents to focus on more complex cases while ensuring faster turnaround times. The AI-driven workflows consistently maintained a 100%accuracy rate, ensuring that customers received timely and reliable updates on their claims.
This digital transformation not only enhanced operational efficiency but also improved customer satisfaction, setting a new benchmark for service excellence within the organization.
About the enterprise
Industry
Insurance Services
What do they do?
The company offers a comprehensive portfolio of General Insurance products designed to meet diverse individual and business needs. As of March 31, 2023, it reported a Gross Written Premium (GWP) of over ₹10,000 crore. With 213 offices nationwide, the company boasts a strong multi-channel distribution network comprising over 76,000 licensed agents, 550+ brokers, and multiple bancassurance partners. Supported by a workforce of more than 8,200 employees, this leading insurance provider has proudly served over 5 crore customers to date.
More case studies

Take the leap towards innovation with Rezo.ai
Get started now







